Update: 03/13/2020
Yesterday I had a Linq cardiac loop recorder implanted into my chest.
We drove up Wednesday night and stayed in a hotel because Toledo is 3.5 hours from our home and we didn’t want to have to get up before the sun to make the drive… especially because that is around the time I am vomiting every morning.
We arrived at the hotel at 9:50. That’s exciting only because the pool at this hotel didn’t close until 11:00! So for the first time in a REALLY long time, I was able to take a dip in the pool. I didn’t swim, but I did stand in the hot tub up to my waist and chat with a gentleman for 10 minutes or so and then I went and sat on the steps of the pool with the water up to my waist to cool off while my dad swam laps. With a fentanyl patch on my back, I can’t really submerge in the water. We covered it with a aquaguard/tegaderm, but we haven’t had the best luck with the tegaderm keeping the patch on when I am submerged in water so I try to keep the water level below the patch.
After we swam, we went back up to the room and dad showered and I threw my clothes back on so we could run to Meijer for some body wash (I was out at home so I couldn’t pack any), dad could get an emery board. And of course, we bought other things we didn’t need because who doesn’t walk into a store and buy things they don’t need?
After our trip to Meijer, we drove to the Wendy’s we saw just off the highway only to find that it closed @ 10PM. We did a Google search and found another Wendy’s that was open until 1AM because it was 11:30PM at this point and didn’t want anyone to spit in/on our food because we showed up while they were in the process of closing (I am joking. I hope no one would do that!). When they handed us our food, I opened the bag to make sure we got everything we ordered (dad’s double cheeseburger with only ketchup, mayo, and extra cheese and french fries and my french fries) and it was all correct and I noticed immediately that nothing in the bag was hot… so we had to wait to until we got back to the hotel where we could use the microwave in the room to heat up our food before we could eat.
When we finally ate, it had been nearly 24 hours since I had eaten and there was not a single point throughout the day… not even at the end, right before we ate, that I felt hungry or that my stomach growled.
My dad didn’t sleep much at all Wednesday night. Despite what he thinks, he got a few minutes of sleep here and there. I was awake all. night. long. Being awake all night allowed me to hear his occasional snoring letting me know when he was able to sleep and when he wasn’t. Not that I was ever jealous or bitter… Again, I am joking. He does so much for me… Including driving me 3.5 hours away after having worked all day. He deserves every minute of sleep he can get.
Thursday morning, when we arrived at the hospital, they screened us at the door for Coronavirus by asking us a series of questions and then based on our answers, they decided if we could continue on to our appointment or if we (and subsequently the person who screened us because they had now been exposed) needed to be quarantined. We then had to carry the determination around with us on a specific sheet of paper.
Once it was determined that we didn’t have the coronavirus, we proceeded to the Heart and Vascular department so I could check in. After being checked in, it was only a couple minutes before they called me back.
On our way back to pre-op, they gave my dad a buzzer similar to the ones restaurants give you when you get when you go out for dinner and you have to wait for a table to become available. They told him to sit in another waiting room and they would page him when I was prepped for surgery and he could come back and sit with me.
We proceeded on to pre-op (which I later found out was also post-op). Pre-op was a small wing with 5 or so beds aligning both walls with curtains surrounding each bed. The nurse showed me to my bed and asked me to trade my bra, tank top, and sweatshirt for a hospital gown (I was allowed to keep my own clothes on from the waist down). After I changed, she showed me to the bathroom and asked me to pee in a cup so she could do a pregnancy test. Surprise! I’m NOT pregnant! It’s hard to be pregnant when you aren’t having sex. Which is E.X.A.C.T.L.Y. what I told the nurse. She then responded by asking if I had ever seen Jane the Virgin the TV show. I told her I hadn’t. She told me it’s about a virgin girl who goes in for a routine procedure only to be mistaken for another patient and be inseminated. No one realizes the mistake until the girl realizes that she is pregnant several weeks later. I was not and still am not sure exactly what kind of point she was trying to make by telling me all of this…
Anyway… After all of that, she paged my dad, letting him know he could come sit with me.
Shortly after he came back a rep from Medtronic came back to show us the heart monitor they would be implanting in my chest and walk us through setting up the transmitter when we get home.

After she finished walking us through everything, Dr. Grubb came over and drew on my chest to show us where the device was going to be placed. After he left, within 2 or 3 minutes, the transport team arrived to take me back. Dad gave me a hug and a kiss and then they wheeled me away.
After we arrived in the operating room they asked me to take my left arm out of my gown and then lay down with my head turned to my right side. They arranged my gown so that left breast was no longer covered but my right breast was. They then scrubbed my chest with iodine. While they waited for that to dry, they began building a “sneeze guard” as they called it. Essentially, there was a halo that hovered over my face, and they used it to drape blue towels off of. These towels blocked my view of the incision site. They were kind enough not to drape towels from my right breast to my right shoulder so that I was able to see the right side of the room and not feel so claustrophobic. They also had a really nice gentleman there just holding my hand and talking to me to keep me distracted.
Back Story:
Dr. Grubb and his team decided while they were requesting approval from my insurance that they were going to sedate me because we have had issues with local anesthesic wearing off during procedures. So where his patients normally get to choose if they would like to be sedated or not, they decided for me, and I am ok with that.
Back to Our Regularly Scheduled Programming:
When Dr. Grubb came in the room, he teased his team for washing his drawing off with the iodine because he had to redraw it.
He then said “You’re going to feel a pinch and some burning after that.” And that’s when I started to panic and said “NO! NO! NO! You’re suppose to be sedating me! I haven’t been given anything! STOP! NO!”
He quickly apologized while someone administered versed & fentanyl to sedate me. He also explained that because of the “sneeze guard” he couldn’t see my face so he was unable to see that I was not sedated.
I am not entirely sure what the versed and fentanyl was suppose to do, but it sure as heck did not sedate me. I was completely conscious and aware the entire time. I was not loopy or high. I just felt a little tired. But because the versed and fentanyl did not sedate me… that means that I was awake for the entire procedure.
I think I could have dealt with being awake for the procedure if the local anesthetic had worked, but that didn’t work either…
Which means I felt E.V.E.R.Y.T.H.I.N.G.
I felt the incision…
I felt the insertion of the device into my chest…
and I felt him suture me closed.
I am thankful that it was a very quick procedure.
And I am even more thankful that they had a very kind man on my right side holding my hand and talking to me.
After the sutured me up, they rolled me back to the pre-op/post-op area where I monitored for a couple of hours before we made the 3.5 hours drive home.
So what comes next?
From the cardiac side of things… we wait for this to heal and then after I am getting consistent nutrition, we will continue along the path towards fixing the SVT.
I found out last week that there was a miscommunication (or lack of communication) when we were discussing the possibility of a feeding tube with my G/I. When my dad and I met with my G/I to discuss this possibility. We thought that they would place a nasojejunal tube (also known as a NJ) and send us home to see if the vomiting stopped and my symptoms improved and if it did, then we would schedule the surgical tube placement. Unfortunately, that’s not the case. They want to admit me for a week for the tube trial.
They will admit me into the hospital, place a temporary tube called a nasogastric tube (also known as a NG) tube up my nose, down my throat, and into my stomach. They will then run formula and see if I can keep it down. If I do, they will pull the NG and place a surgical tube in my abdomen (called a PEG) that will go directly to my stomach so I can run formula and much more importantly, meds, at home.
If the NG doesn’t work… If I am throwing up the feeding tube formula, then they will pull the NG and put another tube up my nose, down my throat, through (passed) my stomach, and into my intestines called a nasojejunal tube (also known as a NJ). Once food makes it into your intestines, you cannot throw it up. So that is a plus. They would run the formula just as a precaution. Then they will pull the NJ and place a permanent tube in my abdomen directly into my intestines so I can run formula and meds into my intestines.
Unfortunately, because we will be in Chicago for a week… not only will I be missing work for a week, but so will dad also be missing work for a week because he will be staying with me for a week.
But that also means that neither of us will be able to care for my brothers (they both have fetal alcohol syndrome) for at least a week…
Since we lost my (step) mom 9 years ago… we don’t really have very many people we are close to. We only see her family once in a blue moon because my step brother wants nothing to do with us. He is is hurting and in a bad place… Understandably, my step family feels like they cannot invite us to holiday dinners or anything of that nature because they are all he has left. And we certainly understand that & don’t blame them. It does make it really lonely though because our only other family nearby is my dad’s mom and because she is a snowbird, she is only close by for 6 months of the year.
Which makes it really hard when you need someone lean on…
We have been very fortunate that Dad’s friend of more than 20 years, Pat, has been a HUGE help by taking my brothers for a day or two here and there when we have had appointments in Chicago or Toledo and needed someone to look after my brothers, but it would be too much to ask him to look after the boys for a week.
So we have been trying to work out the logistics, but it sounds like my grandpa (dad’s dad) and grandma (dad’s step mom) are going to watch my brothers for us while we are in the hospital. They live 8 or so hours away from us so we don’t see them very often, but it means a lot that they are willing to help!
I am waiting to hear back from my doctor as to when they would like to admit me. It seems silly to admit someone who is reasonably stable and only needs nutrition when all of this stuff with the coronavirus is going on… But what do I know?
Once we get the feeding tube placed, and my body is getting consistent nutrition, we will proceed with an electrophysiology study & ablation for my heart and the periacetabular osteotomy for my left hip.
That’s all I have to update on for now. I hope everyone is staying safe and healthy!
~Trinket
Update: 02/15/2020
It has been a really crappy week.
A week ago today (Saturday, February 8th) dad and I spent 5 hours in the ER because I am still throwing up.
When you throw up (for a lack of a better way of explaining it) your body purges potassium, among other vital vitamins & nutrients, along with stomach’s contents. This isn’t a big deal if you have a simple stomach bug, but when you are throwing up every single day, your body never has the chance to try to recuperate…
Because I have been vomiting just about every single day for 11 weeks now, my body has not been able to recuperate. So we have had to make trips to the ER for fluids and potassium. I tried to see my primary care doctor (PCP), but she can’t see me until June 11th. No you didn’t read that wrong. She can’t see me for 5 months. Pretty absurd huh? I don’t know how anyone is suppose to get the care they need if they can’t see their PCP for 5 months.

Anyway… on Monday, I had the brain CT without contrast. While I was there I asked them to please put the scan as well as the CT with and without contrast of my abdomen and pelvis from December 13th and the x-ray of my abdomen and pelvis from December 17th. I filled out the necessary paperwork while I was waiting to be called back. After the CT, I asked how long before the CD would be ready and was once the CT was finished processing, it would take 20 minutes to create the disc. We decided that because we didn’t need it until Thursday, we would come back to pick it up when it was ready… later in the week.
Come Wednesday, I still hadn’t heard anything from anyone in regards to the CD so I called to check on it. The woman who answered the phone once I was transferred to the radiology department told me that the machine they use to create the CDs had been down since Sunday and there were no signs of it being repaired any time soon.
I started to panic a little bit. The woman on Monday never once mentioned the machine being down and I needed that CD in less than 24 hours… and I politely told her as much. She asked me if I would like to speak with her manager. I said please and thank you. Unfortunately her manager was not in her office so I had to leave a message, but her manager called me back quickly.
I think there must have been some confusion though because the manager assured me that the machine was in fact up and working and that she was creating the disc that I needed and it would be ready for me to pick up when I got off of work…
Afterwork, Dad and I drove across town to pick up the CD. The same woman who checked me in on Monday, greeted me at the front desk of the radiology department. I told her I was there to pick up the disc with my scans on it and she told me that they don’t create the discs until you are there to pick them up… Once again, I was VERY confused. It’s as if the left hand doesn’t know what the right hand is doing. I asked her to please just take a look because I spoke to the supervisor on the phone and she promised me it was already created.
Low and behold not only had they already made the disc… they made they disc on Monday and because no one bothered to check, they remade it before I came to pick it up on Wednesday!
…all of that to say, I got worked up and stressed out over absolutely nothing.
On Thursday, I saw my GI doctor. he reviewed the disc I brought with me. My brain CT didn’t show any changes in my ventricles.
After further discussion we determined I have gastorparesis (delayed emptying of the stomach). With a normal human, food isn’t digested in the stomach, it’s mashed so the intestines can digest it. With normal people, food only stays in the stomach for a MAX of four hours. With gastroparesis or delayed emptying, food can stay in the stomach for much much longer because the stomach is not mashing it like it should… but once the food is in the stomach for too long, it starts to rot because of the stomach acid, so it comes back up. Which is the issue I am having… I’m puking up chunks of undigested food because my body is like “Hello! This food is rotting in here! Time to eject!”
So what does our treatment plan look like going forward? We are doing a very thorough MRI to make sure there isn’t a blockage. Then we are starting a medication called Prucalopride that is used for constipation but has shown some success in improving gastric emptying of the stomach speeds/times. If that doesn’t work (because there is only one medication legal in the US) they are putting a feeding tube in.
Receiving a gastroparesis diagnosis and finding out a feeding tube might be in my near future weren’t even the most disheartening part of the day… at Rush Medical, after you meet with your doctor, you go to a “check out” station where they schedule your follow up appointment (if the doctor wants to see you again) and put in any orders the doctor may have requested. When we went to schedule our follow up appointment, the next available appointment wasn’t until the first week of April. The thought of getting this MRI done and then having to vomit every single day for several weeks before we could see the doctor so he could review the MRI and prescribe the medication literally brought me to tears. I cried right there trying to check out…
The receptionist was very sweet. She tried her best to reassure me that he would squeeze me in once the MRI was done, but when the vomiting started in late November I was emailing him several times a week and they couldn’t get me in any sooner than the appointment I was able to schedule originally which was 8 weeks out.
Anyway… yesterday, I was able to call and schedule the MRI for 2/24. After we received the results from that, I will trial the medication. Hopefully that medication will work well and there will be no side effects or reactions!
I will keep you all updated!
~Trinket
Update: 01/24/2020
Yesterday I had two appointments in Chicago. One with a new endocrinologist and one with my GI.
As of yesterday, it has been 8 weeks since my food and meds began coming back up undigested. Throwing up my meds also means throwing up my steroids and that can be dangerous… life threatening even. And that is why I reached out to my local GI for help keeping my steroids down. Unfortunately he did not have anything helpful to offer so I was referred out for a second opinion in Chicago at Rush where I already see several doctors.
This new endocrinologist had a good idea (using prednisolone which is a liquid steroid they can flavor. It’s most commonly given to children who cannot swallow pills.), but he did NOT have very good bed side manner. I spent a majority of the appointment crying… I’m not sure if we will be seeing him again.
As I mentioned before, we also saw my GI doctor. At the beginning of the appointment, he was pretty much convinced that constipation is the cause for my vomiting… that if I was so backed up with poop, of course I was going to vomit because there was no where for the food I was eating to go! but after further discussion, he realized that more than likely is not the case.
From the moment that I first met him, he has been hyper focused on the fact that I do not poop daily or even every other day like most people (or people should). Instead, prior to vomiting, I was pooping every 3-4 days. There could be a lot of reasons for this, but the biggest culprit is severe pelvic floor dysfunction. I’ve done more than a year of pelvic floor therapy and we have seen absolutely no improvement, but we aren’t giving up. But here’s the thing… I was still pooping every 3-4 days until 2-3 weeks AFTER i started vomiting… at which point I started pooping evert 7-9 days. I assume this is because I am puking up a majority of my food and meds (meaning not a lot is getting passed my stomach and into my intestines to be pooped out).
It was after we talked about how I cannot take my morning meds or eat breakfast or eat lunch or eat at work because it causes me A LOT of abdominal pain. About how I have to wait until I get home after 5 most days to eat. It was this that caused him to have me lay down on the exam table so he could examen my abdomen. After examining my abdomen, he was surprised to find that despite having not pooped in 6 days, my abdomen was not as firm or bloated as he expected it to be. To confirm his suspicions he ordered a KUB (x-ray of the kidneys, ureters, and bladder but it covered from your collar bone to your pubic bone so it allows doctors to see your entire digestive tract). The KUB showed that while there was a moderate amount of stool in my rectum, I was not impacted. My GI feels that this is consistent with severe pelvic floor dysfunction. He also said that because I am not impacted the constipation would not be the cause of my vomiting.
It was at this point that my dad mentioned that I have been exhibiting symptoms that my intracranial pressure has been more elevated than usual… things like my vision being so blurry that I cannot see people’s faces despite having my glasses on, increased head pain, etc. My GI doctor said that it is very possible that the increased intracranial pressure could be causing dysmotility. To confirm that suspicion, he ordered a CT of my brain without contrast. We will do that at home.
I will update when I have the results.
~Trinket
Update: 01/10/2020
I don’t even know where to start… Let’s just say that 2020 is not off to a great start.
…but before we dive into what a shit show 2020 has been, I have to back track a little bit.
On 11/28/2019, I started vomiting approximately 12-16 hours after I eat… and my food comes back up undigested. In two days (on Thursday, January 30th) I will have be vomiting my undigested food for 9 weeks. It’s been nothing short of miserable.
Unfortunately, my GI (who is based out of Rush University Medical in Chicago) has been in and out of town. When I was finally able to get ahold of him, he requested a CT with & without contrast of my abdomen and pelvis. I called around to all three hospitals in my area and both of the “private” imaging centers (an imaging center not affiliated with a hospital) and none of the imaging centers could get me in for three weeks. When I asked each center if they had any suggestions, they all suggested that I have the CT done in the ER.
On Friday, December 13th, we made the trip to the ER. Thankfully, there were only a couple of people in the waiting room.
*Side Track* One of the many perks of the hospital I go to is that they have what they refer to as a “quick lane” where patients who need stitches, have (non-severe) broken bones, need tested for strep, etc… this is where the patients that probably should have gone to urgent care are seen. This “quick lane” system helps patients who need to have blood drawn, imaging done, receive fluids and such via IV, for more emergent reasons get into the ER more quickly.
Anyway… back to the point. We were taken back pretty quickly. They drew blood. I was dehydrated as we expected. They gave me a couple of bags of fluids and we did the abdominal and pelvic CT with & without contrast. I was then sent on my merry little way.
Unfortunately, we returned four days later on December 17th because when they released me on the 13th, they told me if my symptoms worsened or I started running a fever, to please come back. Well… low and behold, I started running a fever on Sunday night. It broke in the middle of the night on Sunday, but came back with a vengeance Monday morning… So we went in to the ER on Monday afternoon. Unfortunately, they were SLAMMED because one of the other ER’s in the area was was not accepting patients because their computer system… so we sat in the waiting room for *at least* FIVE hours before making it back to a bed in the ER where we spent another SEVEN hours. During our 12 hours in the ER, I saw three different doctors and never once did I see the same doctor twice. It was insanely frustrating.
The first doctor I saw in the waiting room. He pulled me into a private room to get my vitals and ask me what made us make a trip into the ER. Once I finished telling him that my food had been coming back up undigested for quite some time, he told me that they would likely admit me for a full GI work up. I told him that wasn’t ideal as I had a cardiology appointment I had been waiting 18 months for the following week. He was hopeful the admission would not be more than a couple days… and at least this way, we could get to the bottom of things.
The second doctor I saw shortly after we were taken back into the ER and given a bed. She ordered blood tests, a strep test, a flu test, and a KUB (x-ray of the kidneys, ureters, and bladder).
The third doctor I saw was several hours later after all the results had come back. He told me that my potassium was really low (SURPRISE! that’s what happens when you throw up a lot!) and I had strep throat. Everything else was ok. No blockage or impaction. He ordered IV potassium, 2 bags of IV fluids, and a IV antibiotics.
When we asked about the 3rd doctor about the 1st doctor’s admission plan, he said that because I have an established GI doctor, I should follow up with him instead… Despite the fact that the earliest available appointment was 01/23/2020…
There is a lot more to say on that topic, but for now we are moving on.
Yesterday, January 9th, I saw an orthopedic surgeon for my hip pain. Upon arrival his staff took extensive x-rays of my hips. He then reviewed them with us. He was able to determine that I have pretty signficant hip dysplasia. This basically means that the socket portion of the joint is extremely shallow. He said in some adults, this isn’t a problem because we have tendons and ligaments that help keep the ball portion of the joint in the shallow socket, but because I have EDS, my tendons and ligaments stretch more than they should… they do not keep the ball of the joint in the socket. It’s also likely that I have a labral tear, but we will need an MRI to confirm.



This means that I will need a pretty intense surgery known as a Periacetabular Osteotomy (AKA a PAO). During this procedure, they not only grind out the socket to make it deeper, they also remove the socket portion of the joint from your pelvis, rotate it to better aline with the leg/ball portion of the socket, and reattach it with bolts.
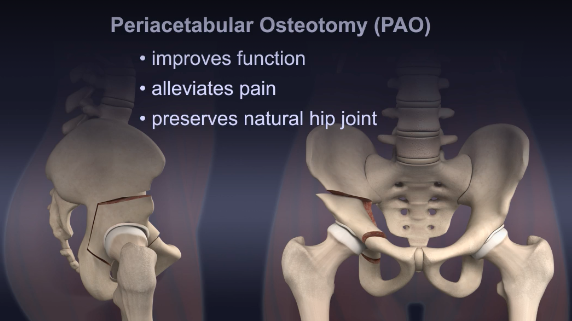
While I will likely need surgery on both of my hips, we cannot do the surgery for quite a while because my food is coming up undigested and I am losing a lot of weight without trying. The surgeon would like me to have several weeks of consistent nutrition under my belt as well as approval from my cardiologist (more on that later) as well as my neurologist (stating that my seizures and intracranial pressure will not be a problem) as I have never been under anesthesia for more than a couple of minutes and this will be a very invasive and extensive procedure. And more then that… the recovery is even more rough. They will obviously do one side at a time. This is because or 8 weeks after the surgery, I cannot weight bare AT ALL. After the initial 8 weeks, you take the next 4 weeks slowly weaning off the crutches. Once you are off the crutches you work with a physical therapist for several months on rehabilitating your hip.
Unfortunately, we cannot move forward with this surgery until I am getting consistent nutrition… whatever that may look like.
That’s all for now!
~Trinket